by Edward Nguni
Imagine falling ill with recurring fever, joint pain, and night sweats, only to be told it might
be flu, malaria, or even tuberculosis. What if none of these were the cause, but rather
something often overlooked?
Brucellosis is a bacterial infection that is transmitted from animals to humans, typically
through the consumption of unpasteurized milk or direct contact with infected livestock. It is
caused by Brucella species, microscopic bacteria that cleverly hide inside immune cells,
making them difficult to detect and even harder to eliminate.
Among these species, Brucella melitensis, which is commonly found in goats and sheep, is
the most dangerous to humans. Once inside the body, Brucella can lead to a debilitating
illness characterised by undulating fever, night sweats, fatigue, joint pain, and serious
complications such as neurobrucellosis or endocarditis.
In 2012, a group of researchers aimed to better understand how Brucella affects people
globally. They sought to quantify the frequency and severity of clinical symptoms in human
brucellosis patients and estimate a disability weight for disease burden calculations. To
achieve this, they conducted a systematic review and meta-analysis of over 25,000 confirmed
brucellosis cases from 57 studies worldwide, utilising generalised linear mixed models to
calculate pooled symptom frequencies, stratified by age and sex. The key findings of their
research are represented in Figure 1 below.
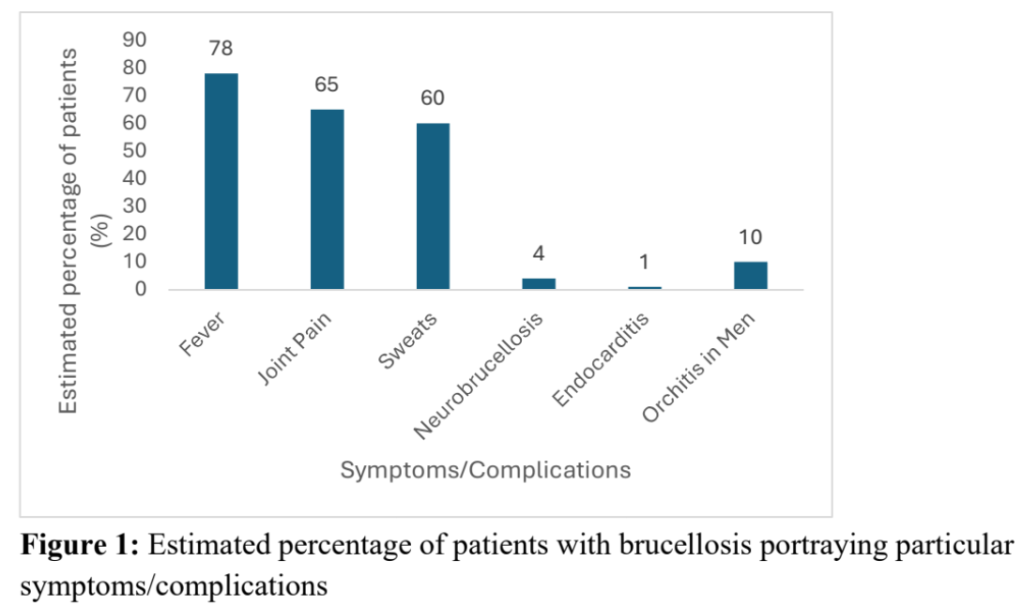
This study highlights the frequent misdiagnosis of brucellosis, particularly in regions where
febrile illnesses are common. It serves as a reminder that neglected zoonotic diseases like
brucellosis continue to pose a serious public health threat.
So, how can we combat this issue? While there is currently no human vaccine available,
brucellosis is preventable. Key strategies include vaccinating livestock—especially goats and
sheep—avoiding raw dairy products, wearing protective gear, and ensuring early diagnosis
followed by long-term antibiotic treatment.
The irony is that while brucellosis is an ancient disease, it remains neglected. Despite being
classified as a Category B bioterrorism agent and recognized globally as a zoonosis, it
receives significantly less attention compared to other infections that present similar
symptoms.
As global health initiatives increasingly adopt a “One Health” approach, brucellosis
emphasises the interconnectedness of human health and animal health, reminding us that
sometimes a fever may originate from a farmyard.
References
Corbel, M. J. (2006). Brucellosis in humans and animals. World Health Organization.
Dean, A. S., Crump, L., Greter, H., Hattendorf, J., Schelling, E., & Zinsstag, J. (2012).
Clinical manifestations of human brucellosis: a systematic review and meta-analysis. PLoS
neglected tropical diseases, 6(12), e1929.
Pappas, G., Papadimitriou, P., Akritidis, N., Christou, L., & Tsianos, E. V. (2006). The new
global map of human brucellosis. The Lancet infectious diseases, 6(2), 91-99.
Leave a comment