By Michaela Kapnias
Think of the blood-brain barrier (BBB) as the foundation of a house. This barrier makes up the roof, walls, windows, and doors, which protect everything inside – your brain. The BBB acts as a physical and functional barrier of the brain, which keeps harmful substances out – like a house keeps out rain and dust – to maintain the brain’s fragile environment. The BBB tightly regulates the entry of substances into the brain, thus significantly restricting drug delivery. So much so, it prevents over 98% of small-molecule drugs, including cancer therapies, from reaching the brain. Now you might be thinking, what happens if chaos transpires in the house and you need something important to be delivered inside? The walls are impenetrable, the windows are sealed, and the doors are closed shut, so what do you do?
A possible solution is using radiotherapy (RT) – a key treatment used for high-grade brain tumours. Irradiating the radiosensitive endothelial cells of the brain vasculature causes the BBB to slightly loosen, allowing an opening for treatment to get in – acting as a transient pry bar on the windows, per se. However, this raises the question of whether RT causes further damage by turning a small leak in the BBB into a systemic flood, thus compromising the BBB integrity. Consequently, a team of researchers from Radboud University Medical Center set out to answer this question in a systematic review and meta-analysis. Their goal was to investigate whether RT increases the BBB permeability and to determine the specific effects of various RT regimens on the BBB.
These researchers began by conducting a systematic search using various medical databases, such as PubMed, Embase, and Cochrane Library. After screening approximately 4 900 studies, they confined their findings to 49 preclinical studies, involving rats and mice, and 20 clinical studies, involving patients. Subsequently, these studies were grouped and compared based on: radiation dose; BBB assessment method; timing of BBB disruption; and type of model.
Furthermore, a meta-analysis was performed on 29 of the preclinical studies, based on treatment and control groups.
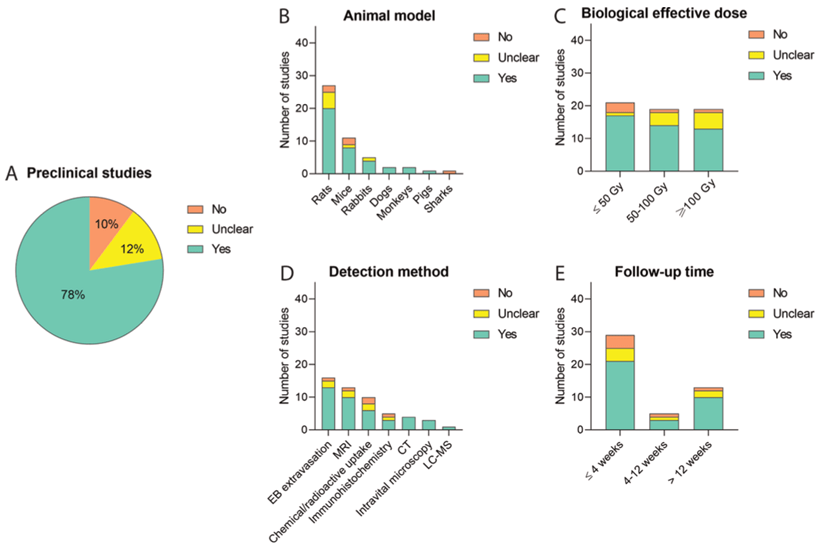
Figure 1: Impact of RT on BBB permeability in preclinical models. A – presence or absence of RT-induced BBB permeability; B – Categorised into type of animal model; C – Biological effective dose; D – BBB disruption detection method; E – Follow-up duration (Hart et al., 2022)
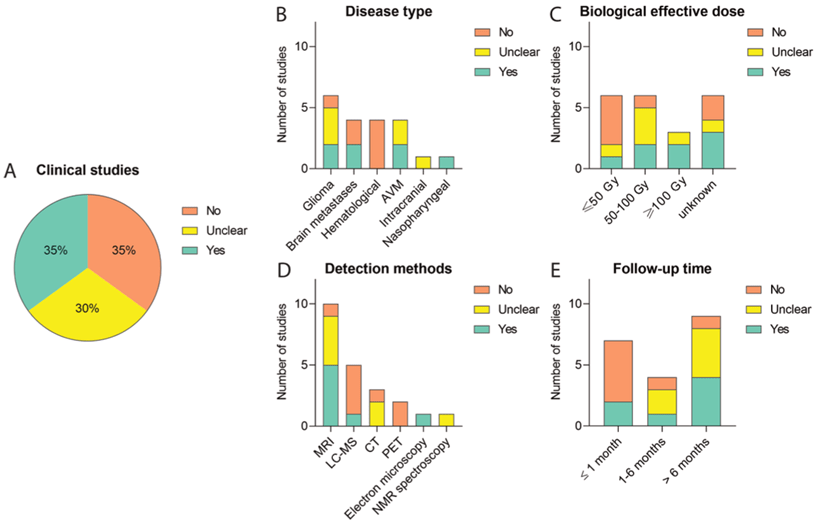
Figure 2: Impact of RT on BBB permeability in clinical models. A – presence or absence of RT-induced BBB permeability; B – Categorised into type of disease; C – Biological effective dose; D – BBB disruption detection method; E – Follow-up duration (Hart et al., 2022).
Evidently, this study determined that RT does, in fact, disrupt the BBB, leading to various implications. For brain cancer patients in particular, a temporary disruption in the BBB may allow more cancer-targeted drugs to reach the tumour. On the contrary, this permeability may also expose the brain to damaging substances resulting in neurotoxicity, inflammation, and long-term brain damage. This raises uncertainty whether the use of RT should be worrying or encouraging. Although not fully understood, this study brings researchers closer to understanding how RT alters the BBB and its possible implications thereof. With the use of this knowledge, scientists can further develop new methods to exploit BBB permeability to enhance drug delivery to the brain, while minimizing severe damage to the BBB integrity.
Reference
Hart, E., Odé, Z., Derieppe, M.P.P., Groenink, L., Heymans, M.W., Otten, R., Lequin, M.H., Janssens, G.O.R., Hoving, E.W. and Vuurden, D.G. van (2022). Blood-brain barrier permeability following conventional photon radiotherapy – A systematic review and meta-analysis of clinical and preclinical studies. Clinical and Translational Radiation Oncology, 35, pp.44–55.
Leave a comment