By Alexander Sittman
“All disease begins in the gut”
– Hippocrates
circa 450 BCE
An Introduction to the Gut-Brain Connection
The Father of Modern Medicine, the great Hippocrates of Kos, is remembered for his uncanny prescience – his theory linking the gut to disease was, if not mechanistically, conceptually accurate. Pretty impressive for a guy who lived nearly 2500 years ago.
I’d like to propose an amendment: not all disease begins in the gut. But research increasingly shows that almost all diseases is influenced by the gut. And, as an extension, your whole self is influenced by the gut – disease-ridden or not. From everyday decision-making to determining the outcome of your embryonic development, your fate is inextricably intertwined with the microbes – of which there are thought to be trillions more than your own cells – that colonise your alimentary lining from entrance to exit. There is no more interesting, nor exciting a new field in the world of microbiome research than the study of the gut-brain axis – a bidirectional relationship explored extensively by (Mayer et al., 2015).
Let’s dive into the world of the miniscule passengers that make you, well, you.
Figure 1: The Gut-Brain Axis. Created in https://BioRender.com
Diving Deeper
The study of the microbiome can be confusing and intimidatingly complex. The thought of dealing with concepts like multilayered enteroneuroendocrine pathways and pronouncing Faecalibacterium prausnitzii terrify even experienced flora fauna fanatics. So, it’s worth outlining what is known before we consider future perspectives. Mayer and colleagues (2015) did just that:
How We Study Gut-Brain Cross-Talk
Most of the methods used to study how gut microbiota modulate the gut-brain axis fall under a few broad approaches – mostly done on mice – and include faecal transplantation, antibiotic manipulation, metagenomics and Germ-Free (GF) animals. The latter of these means laboratory mice raised in sterile conditions with no microbes in or on their bodies. These methods manipulate the microbiome of mouse models so that researchers can study how their physiology and behaviour changes, and extrapolate these results to humans (see Figure 2 below). We’ve discovered some interesting things about neurodevelopment and disease from these experiments.
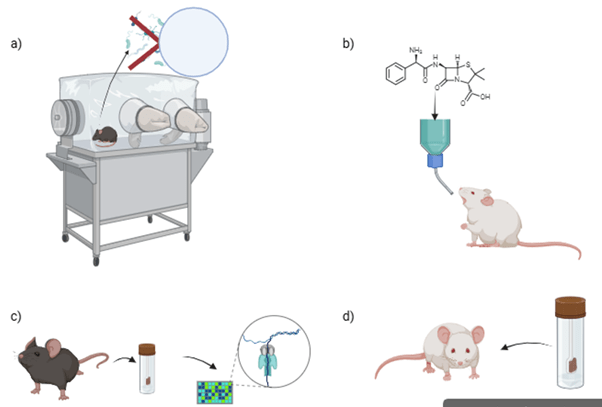
Figure 2: Examples of methods use to study the gut-brain axis in mice: a) breeder isolator used to generate germ-free mice b) treatment of mouse with – in this case – an antibiotic (Penicillin) or pro/prebiotic c) sampling and metagenomic analysis stool samples d) faecal microbial transplant (FMT). Created in https://BioRender.com
Microbes in the Making of a Mind
The gut microbiome plays a surprisingly big role in early neurodevelopment. In prenatal and early postnatal animal models, stress caused considerable changes in the total biomass and composition of gut microbiota. Interestingly, the opposite was also true: the absence or disruption of gut microbes during early life altered emotional behaviour, stress responses, and even brain chemistry. Microbial signals – like short-chain fatty acids and neurotransmitter-like molecules – may shape the developing nervous system, including pathways involved in mood and cognition. While evidence in humans is still limited, these findings hint at a vital gut-brain connection that starts before birth and could influence lifelong psychological wellbeing.
The Microbiome in Normal Physiology and Behaviour
We’ve known for a long time that gut health and dietary habits are fundamental determinants of health. The often-misquoted Ludwig Feuerbach’s 1850 assertion that “Der Mensch ist, was er isst” – man is what he eats – is symbolic of a greater truth: that what we consume doesn’t just nourish our bodies, but profoundly shapes our minds, moods, and even the microscopic ecosystems within us. Today, this symbolic wisdom is backed by science – revealing that our gut microbiome, sculpted by diet and lifestyle, plays a pivotal role in everything from immunity to psychological wellbeing. In essence, we are not just what we eat – we are what our microbes do with what we eat, and how they interact with our nervous and endocrine systems.
“What they do” with it is that they not only modulate, but actually produce a milieu of neurotransmitters (like dopamine, adrenaline, and glutamate) that are intimately involved in the normal functioning of your nervous system – including your brain. Did you know that the gut (under the influence of the microbiome) makes around 90-95% of the “feel-good” chemical, serotonin, you produce? Our gut bugs also directly affect a number of important hormones linked to stress (cortisol) and eating habits (ghrelin, leptin, and GLP-1). Thus, the microbiome influences:
- Feeding behaviours (where and when you eat)
- Taste preferences
- Nociception (your perception of pain)
- Learning and memory
- Stress levels
- Mood and emotion
- Social behaviour
- Sleep patterns
When Stuff Goes Wrong: Gut Microbial Involvement in Neurological Disease
We only really begin to understand the unbelievable importance of the microbiome when we consider that its dysregulation has been extensively implicated in a number of neurological diseases. To name a few: depression, anxiety, autism spectrum disorder (ASD), schizophrenia, Parkinson’s disease, Alzheimer’s disease, multiple sclerosis, chronic pain disorders, and addiction. Changing gut microenvironments have repeatedly been shown to not only correlate with, but be mechanistically involved in the aetiology of these diseases – so what can we do about it?
Where We’re Headed: Microbes and Medicine
While early findings are fascinating, we’re only beginning to understand how the gut microbiome shapes the brain. Further research is needed to uncover how these microscopic communities influence mental health – and whether we can safely tweak them to treat conditions like anxiety, depression, and ASD. Probiotics, prebiotics, and even faecal microbial transplants are being explored as therapies, but results in humans are still mixed. With better studies and personalised approaches, microbiome-based treatments could soon offer a novel therapeutic strategy for mental care.

Figure 3: Examples of existing and proposed microbiome modulation-based therapies for common neurological disorders. Therapies like faecal microbial transplants (FMT) and pre/probiotic treatments are being explored for the treatment of chronic pain disorders, ASD, addiction, depression, Parkinson’s, Alzheimer’s, multiple sclerosis, and anxiety. Created in https://BioRender.com
References
Mayer, E. A., Tillisch, K., & Gupta, A. (2015). Gut/brain axis and the microbiota. The Journal of clinical investigation, 125(3), 926-938. https://dm5migu4zj3pb.cloudfront.net/manuscripts/76000/76304/JCI76304.v2.pdf
Leave a comment